**Medical Cannabis Components and Effects:**
– National Institute on Drug Abuse defines medical cannabis as using the whole marijuana plant or its extracts for treating symptoms.
– A cannabis plant contains over 400 chemicals, with about 70 being cannabinoids.
– Variations in CBD-to-THC ratio in cannabis determine therapeutic effects.
– Treatment with cannabis is challenging due to the numerous active chemicals.
– THC and CBD interact with the endocannabinoid system in the body.
– THC causes psychoactive effects by binding to CB1 receptors.
– CBD does not produce psychoactive effects but influences CB1 receptors.
– Both THC and CBD have potential therapeutic benefits.
– Adverse effects of cannabis use can include impaired cognitive function.
– Different strains of cannabis may have varying effects on medical conditions.
**Medical Uses and Research:**
– Limited evidence supports medical cannabis efficacy for chronic pain and muscle spasms.
– Some potential uses include reducing nausea during chemotherapy and improving appetite in HIV/AIDS.
– Cannabinoids may be recommended for anorexia, arthritis, glaucoma, and migraine.
– Unclear if medical cannabis can mitigate effects of the opioid epidemic.
– Research on medical cannabis health effects is of low quality.
– Lack of evidence for the efficacy and safety of cannabis in treating HIV/AIDS.
– Studies on cannabis and anorexia associated with AIDS are limited.
– Current studies suffer from bias, small sample size, and lack of long-term data.
– Cannabinoids like THC and CBD show promise in treating epilepsy.
– Medical cannabis can be prescribed for various medical conditions.
– Research ongoing to explore potential medical benefits of cannabinoids.
**Adverse Effects and Cognitive Impact:**
– Medical cannabis use may lead to tiredness, dizziness, increased appetite, and cardiovascular effects.
– Other effects include impaired memory, motor coordination, altered judgment, and paranoia.
– Tolerance to effects develops over time.
– Long-term cognitive impairment not believed to occur in adults.
– Recreational cannabis use linked to cognitive deficits, especially in adolescent users.
– Lack of research on long-term cognitive effects of medical cannabis use.
– Early cannabis use may contribute to the development of schizophrenic disorders.
– THC exposure can cause acute psychotic symptoms.
– Cannabis use associated with an increased risk of psychosis.
– Adolescent cannabis use increases psychosis risk.
**Administration and Excretion:**
– Smoking common but not suitable for medicinal cannabis.
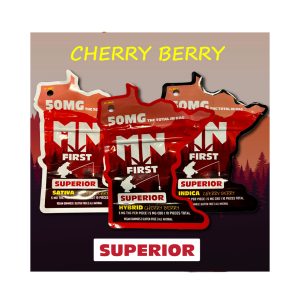
– Concentration of cannabinoids varies widely in different forms of consumption.
– Smoking poses risks from inhalation of harmful chemicals.
– Cannabis vaporizers gaining popularity for perceived reduced harm.
– Cannabinoid medicines available in pill and liquid extract forms.
– THC and CBD metabolites excreted mostly via feces.
– THC undergoes phase II metabolism into over 30 metabolites.
– Approximately 65% of THC excreted in feces, 25% in urine.
– Terminal half-life of THC is 25-36 hours.
– CBD metabolites primarily processed by CYP2C19 and CYP3A4.
**Legislation and Public Opinion:**
– Legal status of cannabis varies globally.
– Some countries have legalized medical cannabis, while others have decriminalized recreational use.
– Regulations surrounding cannabis production, distribution, and use differ.
– Medical cannabis programs require physician approval in many regions.
– Public opinion and legislation on cannabis continue to evolve.
Medical cannabis, or medical marijuana (MMJ), is cannabis and cannabinoids that are prescribed by physicians for their patients. The use of cannabis as medicine has not been rigorously tested due to production and governmental restrictions, resulting in limited clinical research to define the safety and efficacy of using cannabis to treat diseases.
Preliminary evidence has indicated that cannabis might reduce nausea and vomiting during chemotherapy and reduce chronic pain and muscle spasms. Regarding non-inhaled cannabis or cannabinoids, a 2021 review found that it provided little relief against chronic pain and sleep disturbance, and caused several transient adverse effects, such as cognitive impairment, nausea, and drowsiness.
Short-term use increases the risk of minor and major adverse effects. Common side effects include dizziness, feeling tired, vomiting, and hallucinations. Long-term effects of cannabis are not clear. Concerns include memory and cognition problems, risk of addiction, schizophrenia in young people, and the risk of children taking it by accident.
Many cultures have used cannabis for therapeutic purposes for thousands of years. Some American medical organizations have requested removal of cannabis from the list of Schedule I controlled substances maintained by the United States federal government, followed by regulatory and scientific review. Others oppose its legalization, such as the American Academy of Pediatrics.
Medical cannabis can be administered through various methods, including capsules, lozenges, tinctures, dermal patches, oral or dermal sprays, cannabis edibles, and vaporizing or smoking dried buds. Synthetic cannabinoids are available for prescription use in some countries, such as dronabinol and nabilone. Countries that allow the medical use of whole-plant cannabis include Argentina, Australia, Canada, Chile, Colombia, Germany, Greece, Israel, Italy, the Netherlands, Peru, Poland, Portugal, Spain, and Uruguay. In the United States, 38 states and the District of Columbia have legalized cannabis for medical purposes, beginning with the passage of California's Proposition 215 in 1996. Although cannabis remains prohibited for any use at the federal level, the Rohrabacher–Farr amendment was enacted in December 2014, limiting the ability of federal law to be enforced in states where medical cannabis has been legalized.
English
Noun
medical cannabis
- (medicine) Cannabis and cannabinoids that are prescribed by a medical practitioner for their patients.